Difficult doctor (def): a physician that disagrees with, or fails to immediately and graciously comply with, the expressed directive of any nurse manager or hospital administrator. [cf., Policy relating to the Reporting and Disciplinary Procedures for Difficult Doctors]
Many of you are painfully aware that our work environment has recently become–how best to phrase it? Silly? Unpleasant? Challenging? Flat out, batshit crazy? Yes, let’s go with that last one. (See Doctors Without Barbers). And I’m not even going to grace these new policies with any discussion, because they are so imbecilic as to not merit even this amount of attention.
(Doctor, you can’t leave the OR without a jacket. The short, paper one. No, no, no, doctor, not the full length disposable one. Oh my god no, not the full length disposable yellow one, that’s only for isolation and an alarm will go off if you walk out of here with that on. Wear this one, it’s required, but make sure to take it off and replace it with the full length disposable one you had in your hand a minute ago if you step into the hallway with the brown guardrail to tell the family that your patient survived their operation, then take the full-length but not yellow one off and put the short coat back on when walking between the brown railed hallway and back to the OR, then remove the short coat before scrubbing for your next surgery but you can’t don a surgical mask after donning your coat because that would lead to shedding of dangerous skin cells onto the coat, rendering the entire environment a potential health hazard but you can’t go into the OR without a mask and you can’t walk down the hall with a mask dangling on your chest and you can’t walk down that hall to get a mask without the coat on so I guess you’ll just have to not operate any more today, okay? Sorry, doctor, it’s the policy. Have a nice day.)
Those in the business know that I’m not making any of that up. Really.

So, I received the following email recently from our hospital administrator:
Dear Surgical Physicians, Nurses, Techs, and all Operative Colleagues:
As you are aware, our policy for Surgical Attire is based on National Standards, and was developed to ensure our commitment to Patient Safety , which remains our core value. In addition, proper surgical attire continues to be a major focus for both CMS and the State Department of Health. Unfortunately, many of our sister hospitals (as well as hospitals in other systems) have found themselves in a position where physicians and staff members were not following policy to the specified level, and were subsequently placed on periods of Immediate Jeopardy, in which they were at risk of losing their Medicare and Medicaid funding.
We are doing everything we can as a hospital to follow our policy and avoid situations such as that. I am attaching our Surgical Attire policy as a refresher of the expectations at [our hospital]. At the current time, I will remind you that ALL hair is to be covered, including sideburns and hair at the nape of the neck, as well as any facial hair (i.e. mustache). Our strongest recommendation is that to make it most easy for you to comply, surgical hoods should be worn, often in conjunction with a surgical cap, to allow maximum of hair coverage with minimal effort. Mirrors have been added around the operating theater to allow each physician and staff member to best police themselves.
You are all professionals, and your professional obligation is that you will comply with hospital policy. We will be conducting periodic observations to make sure we are compliant. I would ask that all staff please look to help any other physician or staff member who has not noticed that there is errant hair, or other non-compliance with the policy.
I am confident that we, as a hospital, and YOU as the Operative team, will be compliant and successful.
Sincerely,
[name deleted]
Vice President Medical Affairs & Chief Medical Office
So much of what is wrong with our current OR work environment is summarized in this completely nonsensical email. Let’s discuss:
“As you are aware, our policy for Surgical Attire is based on National Standards”–actually, no, it isn’t. It is an ungrammatical, unscientific, ad hoc mash-up of AORN policy recommendations, in-house silliness, and a good bit of complete nonsense. It has no basis in JCAHO or Department of Health standards. It directly contradicts recommendations by many national and international scientific organizations, including the American College of Surgery Manual of Perioperative Care and a recent policy statement by the ACS. There is nothing about it that even approaches a rational scientific basis or accepted standards, national or otherwise. It in no way represents any form of consensus of surgeons, nurses, or surgical technicians, either within the institution or at the level of representative organizations. It was authored by a couple of nurse administrators who haven’t seen the inside of an operating room in decades while sitting in a hospital conference room with a few administrators lacking any clinical insight whatsoever and absent any physician, anesthesiologist, or surgeon who might contribute rational insight into the process; i.e., dissent. The resulting policy was then filed in the Manual of Procedures and Policy without benefit of review by the Chief of Surgery, his designate, the OR committee, or as an agenda item at the surgical departmental meeting. Or by the Chief of Anesthesia, or at the anesthesia departmental meeting. Or by the Chief of OB/Gyn, or at their departmental meeting. Or by the Chief of Orthopedics, or at the ortho departmental meeting. Of course it wasn’t, because the physicians affected would’ve pointed out that the document was nonsense. They would be “difficult.”
“developed to ensure our commitment to Patient Safety , which remains our core value”–unfortunately, your core value has been repeatedly demonstrated to be maximizing revenue. Capitalizing the phrase “Patient Safety” in all official emails does not make it your priority. You have an amazing capacity to re-interpret your institutional commitment to Patient Safety if this proves too expensive. It just so happens that arbitrary rules regarding surgical attire costs the hospital nothing. And by the way, if you truly believe that the type of hat worn by a surgeon or OR nurse is an issue of patient safety, you really shouldn’t be allowed to come to work as a hospital administrator.
“Our strongest recommendation is that to make it most easy for you to comply, surgical hoods should be worn, often in conjunction with a surgical cap, to allow maximum of hair coverage with minimal effort.”–of course, this recommendation makes no sense, which is obvious to anyone who has actually set foot in an OR, and creates a situation in which you will be unable to operate, or keep from sweating into your patient’s wound (recent policy change takes away the ability to control OR room temperature without contacting an administrator), or breathe. We’re just interested in making it “most easy for you to comply.” Comply or die, whatever. Minimal effort.
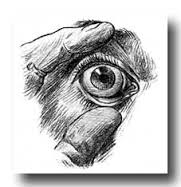
“Mirrors have been added around the operating theater to allow each physician and staff member to best police themselves.”–I have no words.
“I would ask that all staff please look to help any other physician or staff member who has not noticed that there is errant hair, or other non-compliance with the policy.”–Please report your fellow workers to the authorities. You may be awarded the coveted “Employee of the Month.”
And more recently, yet another hospital email regarding this same subject ended with the following threat:
Please review the attached Guidelines for Operating Room Environment and Surgical Attire Policy.
Non-compliance with our policy will compromise the Hospital’s position with the DOH and may lead to financial penalty for the Hospital. For physicians who are found to be in violation of our policy, a ‘non-adherence to policy that compromises patient safety’ note will be placed in the credentials file as part of their OPPE.
So, it’s okay that the OR nursing supervisor is “surprised” to realize that my hospital has no CO2 cylinders available when the tank goes empty halfway through my laparoscopic procedure, which results in no incident report, meeting, or repercussion of any sort, but if I fail to wear a disposable short coat while walking between the OR and the recovery room I will be cited as “compromising patient safety.” A note will be placed in my permanent record.
Seriously.