“The universe is made of stories, not atoms.”
A pioneering work of of “Neuro-Scifi”.
God Bless The Dead by Evan Geller
A pioneering work of “neuro-scifi” and tech start-ups, where Breaking Bad meets American Gods.
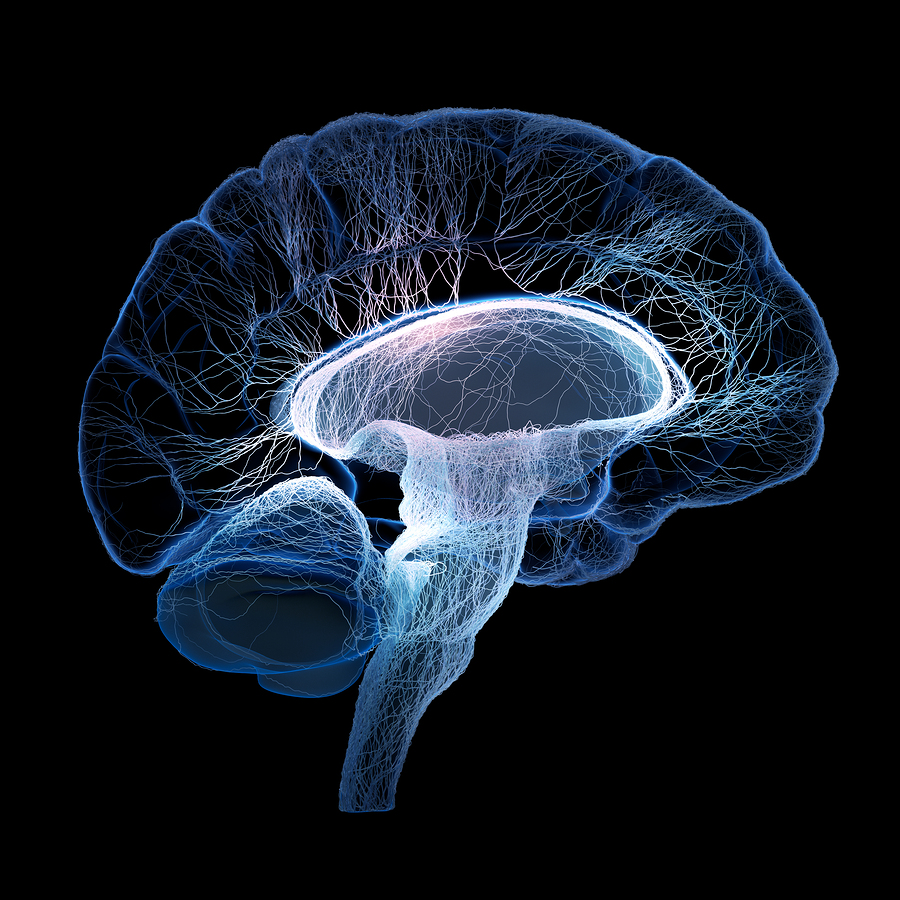
We’re accustomed to thinking of the space inside our heads as private. Our thoughts, feelings and emotions are the landscape of an inner world that only we have access to. All art is about the attempt, however incomplete, to express what lies within to the outer world. Today humankind may be on the brink of changing this most fundamental assumption of our existence, as the techniques of neuroscience, of brain scanning and neural imaging, open up our inner world to scientific investigation. It’s this scientific revolution that forms the backdrop to Evan Geller’s remarkable – and remarkably amusing – debut science fiction novel, God Bless The Dead.
“the first technology to read human brain patterns is deployed as a smartphone app that allows consumers to order a Coke with the power of their mind alone”
Gabriel Sheehan is a struggling young scientific researcher, derailed from the fast-track-to-success by one fundamental problem. His research isn’t producing results. Applying the cutting edge in brain scanning technologies to reading minds in the lab should have been a “no brainer”, but after years of work and tens of thousands of dollars wasted, all Gabriel has to show is a pile of junk data. Inspiration arrives in the form of Helena Fianna, a talented Irish student of astrophysics who seems to hold the key to Gabriel’s research, and to his heart.
Evan Geller skilfully weaves a intriguing tale from three quite different kinds of story. Gabriel and Helena’s romance unfolds with all the whit and wry social observation of a Jonathan Franzen novel. The Sheehan family are a perfect portrait of America’s educated upper middle class, who remain charmed by the chaotic young Irish woman in their midst even once they begin to suspect her mysterious background. Is it normal to discover your fiancé keeps a stolen Duccatti 1199 in a seedy lockup? And that her real name probably isn’t Helena? Of course not, and Gabriel will be dragged far outside any normal life by his strong willed new wife.
Gabriel’s research project is in one sense a science fiction story. But it’s the kind of sci-fi which understands that scientists aren’t mad inventors in secret bunkers, but the founders of multi-billion dollar businesses. Gabriel and Helena realise that to find patterns in human thinking they need to scan humans en masse. They have the technology, what they lack is the marketing. And so, exactly as would happen in this day and age, the first technology to read human brain patterns is deployed as a smartphone app that allows consumers to order a Coke with the power of their mind alone. And at the same time report back invaluable data on human thought patterns to Gabriel and Helena’s new company.
The product of this mass data collection is “the salmon”, a database of universal human thought patterns that will make many people immensely wealthy, and attract the attention of some powerful factions, from the corporate boardroom to the NSA itself. But, God Bless The Dead’s core story is more mystical than science fictional. Eagle eyed myth hunters will recognise The Salmon of Knowledge from the Fenian cycle of Irish myths, one of many references to these ancient stories scattered like gems in Geller’s novel. That Helena Fianna is much more than she seems is apparent from early in the story, but just how much more is a mystery that unfolds, step by expert step, in the narrator’s surgically steady hands (Geller is in fact an accomplished surgeon, when not filling pages with words).
“a rom-com take on Breaking Bad, mixed with the urban fantasy of American Gods”
God Bless The Dead is a big book, and this reviewer’s only substantial criticism is that it’s pace is sometimes a little slow. Geller is a very skilled writer of quick fire dialogue. Scenes between Gabriel and Helena blaze past as they affectionately eviscerate each other in the way that very intelligent people in love commonly do. When NSA agent Chuck Parnell appears to investigate the eves dropping capabilities of Gabriel’s research, the reader is left with the absolute conviction that, yes, the NSAs top agents really would be annoying, fast talking geeks that just never go away. But Geller occasionally over deploys this gift of the gab, dragging down the pace of his story with scenes that could be reduced to a few lines of summary.
This criticism aside, God Bless The Dead is a novel of remarkable storytelling skill and panache. It’s episodic structure is very much in the HBO style so popular in television today. At points Geller’s novel feels like a rom-com take on Breaking Bad, mixed with the urban fantasy of American Gods. God Bless The Dead succeeds in feeling contemporary while capturing a mythic atmosphere, wrapping both in a tale of science fictional intrigue. It’s a rare combination, that many reader will greatly enjoy.
Advertisementshttps://c0.pubmine.com/sf/0.0.3/html/safeframe.htmlREPORT THIS ADAdvertisementshttps://c0.pubmine.com/sf/0.0.3/html/safeframe.htmlREPORT THIS AD
Share this:
Published by Damien Walter
Writer and storyteller. Contributor to The Guardian, Independent, BBC, Wired, Buzzfeed and Aeon magazine. Special forces librarian (retired). Director of creative writing at UoL, published with OUP and Cambridge. Currently travelling the world and writing a book. View more posts